In 2017, the Molecular Biophotonics Laboratory – led by ME professor Jonathan Liu – pioneered a now-patented technology called open-top light-sheet microscopy. The 3D imaging method enables clinicians to see a complete microscopic view of tissue specimens, such as a biopsy or surgically removed tumor, which could improve how diseases are diagnosed and treated.
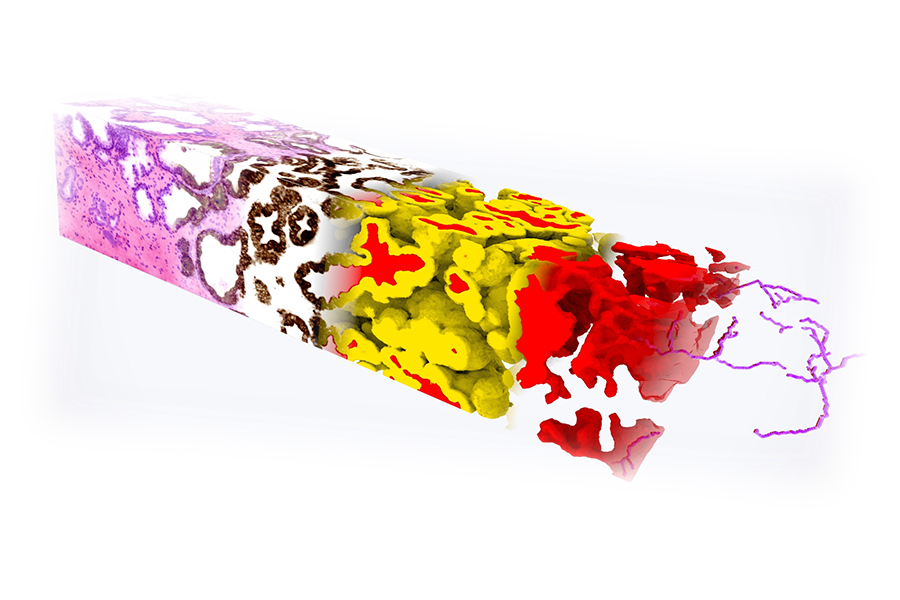
A 3D pathology dataset of a prostate biopsy stained with a fluorescent analogue of H&E. Deep learning-based image translation was used to convert the H&E dataset into a synthetic dataset that looks like it has been immunolabeled to highlight a cytokeratin biomarker (brown) expressed by the epithelial cells in all prostate glands. In turn, this synthetically immunolabeled dataset allows for accurate 3D segmentation of the prostate gland epithelium (yellow) and lumen spaces (red). Quantitative features derived from these segmented 3D structures are used to train a machine classifier to stratify between recurrent versus non-recurrent cancer. Reference: W. Xie et al., Cancer Research, 2022.
“What gets people excited at the end of day is how this is going to impact patient care,” Liu says.
Currently most pathologists use a 2D method of imaging tissues, which involves cutting a small percentage of the tissue sample into thin slices and staining and viewing them on glass slides under a standard microscope to determine their level of abnormality. This traditional method allows them to see only a small fraction of a sample in 2D and can lead to inaccurate diagnoses and suboptimal treatments, such as a person receiving radiation or surgery although their cancer only requires periodic monitoring.
The nondestructive 3D imaging method developed in Liu’s lab can rapidly image 100% of certain tissue samples such as needle biopsies and keeps the tissues intact so that they can be used for other tests.
The open-top light-sheet microscopy device shines a sheet of light that optically “slices” through samples that are made transparent through a simple and gentle “optical clearing” process. All of the optical components in the microscope are positioned below a glass or plastic sample-holder platform, allowing for rapid and simple imaging of a wide range and number of clinical specimens. Researchers in the Liu lab then develop computational analysis methods to delineate and quantify key tissue structures to determine cancer aggressiveness.
In 2022, the researchers published a study in the journal Cancer Research showing that 3D pathology could enable more accurate identification of aggressive prostate cancer cases that could recur within five years. Prostate cancer is the most common cancer and the second leading cause of cancer death for U.S. men. Because it can be slow-growing, identifying which cases require monitoring or treatment is important. 3D pathology could also be used in other cancer treatments, such as predicting which cancer patients might respond to immunotherapy.
“Better ways to determine which drugs a patient should take is a huge need,” Liu says. “Machine learning can find needles in a haystack that are hard for human observers to see within our large 3D datasets, which can be important for determining the aggressiveness of a disease or how likely the disease will respond to specific treatments.”
Alpenglow Biosciences is a company co-founded by Liu that commercializes the lab’s technologies, such as the researchers’ newest and most versatile microscopy system, a hybrid open-top light sheet microscope. It can perform rapid, automated imaging of multiple specimens at various levels of magnification. Liu’s lab published this latest microscope system in a paper in Nature Methods in May.
This year, the lab is scaling up its prostate cancer research to include collaborations with universities across the country and even internationally – pointing to a growing awareness and interest in open-top light-sheet microscopy.
Projects include National Institutes of Health-funded research with Emory University to combine 3D tissue imaging with AI-powered diagnostic imaging to better determine prostate cancer risk and working with the University of Pennsylvania to compare the 3D pathology of specific populations to develop tailored AI methods. In October, the lab will host researchers from the University of Oxford and train them on 3D pathology methods. Through a project funded by Prostate Cancer U.K., the lab aims to ship a microscope to Oxford in 2023 so that U.K. researchers can use it to image tissues.
“Oxford has one of the largest collections of prostate tissues in the world from patients in which outcomes are being tracked for 10 to 20 years,” Liu says. “Working with Oxford could really help us to show the value of our 3D pathology methods for predicting which patients have lethal versus slow-growing disease.”
In addition, Liu is working with UW Medicine to create a hub for 3D pathology, and the lab will conduct smaller-scale clinical studies to show the feasibility of the 3D imaging method. The goal is to use AI to assist pathologists’ final diagnosis and to guide oncologists’ treatment recommendations.
Originally published October 31, 2022