By Andy Freeberg

Video by Samantha Bremner, UW Bioengineering
If the video above looks a little like a heartbeat, that’s because it is one. This bit of engineered heart tissue, slightly longer than a grain of rice, contains roughly a million cardiac cells all contracting and relaxing in concert, exactly the way they do inside our chest.
Though miniscule, the tissues hold enormous promise for understanding one of our body’s most essential organs. Heart disease is the world’s leading cause of death and is only one of the many conditions and medical complications that affect the heart and impact human health.
Any given week in UW’s Cell Biomechanics Lab researchers might engineer a few dozen of these beating heart tissues. The lab, led by mechanical engineering professor Nathan Sniadecki, is specifically interested in the mechanics of heart tissue – the tightening and stretching of cardiac muscles – and the fundamental relationships between the cellular structures and their functions within the tissue.
“The heart is dynamic - it has an incredible ability to adjust itself,” says Sniadecki, who’s also an associate director for the UW Medicine Institute for Stem Cell and Regenerative Medicine. “Learning more about how and why it makes those adjustments could impact everything from cardiac treatments and drug screening to sports medicine and space travel.”
Each time I see these beating tissues, I’m still inspired by the awesomeness of our biology. But I also see a world of possibility there for impacting people’s lives, and that’s the most romantic part of all.
How to grow a heart (tissue)
The process of engineering a living, beating heart tissue starts with a set of human stem cells that are first urged to develop into cardiac muscle cells. Those cells are carefully and methodically mixed with a cocktail of other cells, proteins and enzymes in a sort of biological Jell-O mold, into which a pair of little pillars is inserted. The pillars are just over a quarter of an inch (eight millimeters) apart.
With the ingredients all in place, the tissues just need time to develop. Within a day the cells start to condense and become fibrous. After about two weeks comes the miraculous moment when the cells start to contract in unison and a heartbeat emerges.
A plate of 12 beating engineered heart tissues. Researchers can measure the strength of each heartbeat using magnets embedded in the pillars they’re suspended from. Video courtesy of Nate Sniadecki / UW ME
“The first time I saw it, I thought it was the coolest thing I’d ever seen,” says Samantha Bremner, a graduate student in bioengineering who works with Sniadecki in his lab.
Bremner has produced hundreds of these tissues, mastering the small details that ensure each one is consistent enough to use for research.
With the help of tiny magnets embedded in the pillars that the tissues are suspended from, researchers can precisely measure how strong and fast each heartbeat is and monitor the tissue’s condition. If the tissues are healthy and regularly cared for, they can continue beating for months.

A series of miniature engineered heart tissues suspended across pillars about a quarter of an inch apart. Within each tissue is a 3D assemblage of cardiac muscle fibers (inset). Image courtesy of Nate Sniadecki / UW ME
Secrets of the heart
The engineered tissues are part of a current boom of research that takes advantage of induced pluripotent stem cells – stem cells derived from a Nobel Prize-winning technique where adult skin or blood cells can be reprogrammed into other cell types. In the case of creating heart cells, the research team believes the tissues are useful for a range of new studies of diseases, drugs and medical conditions.
One of the most promising applications of engineered heart tissues is rapidly screening for the potential effectiveness, or side effects, of new drug treatments. Traditionally researchers use lab mice and other small mammals for these kinds of safety tests, but these heart strings offer another way to look for risks that better approximates a human subject. For example, this past year as doctors raced to consider treatments for COVID-19, Sniadecki and colleagues tested giving the novel coronavirus to their engineered tissues and experimented with how different drugs worked against it.
One specific disease that interests Sniadecki and Bremner is Duchenne muscular dystrophy, a genetic condition in which muscles slowly degrade over time because they can’t produce a protein called dystrophin. People with this condition are typically in a wheelchair by age 15 and often don’t live past their 20s because their hearts give out. The UW research team has created engineered heart tissues using stem cells from people with this condition and observed how the lack of dystrophin damages the muscle fibers.
Hearts in sport and in space

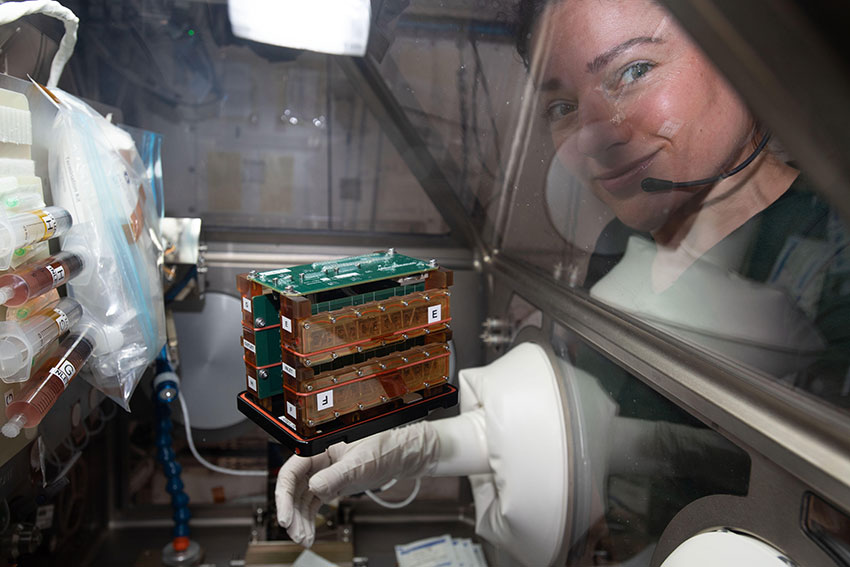
Astronaut Jessica Meir “feeds” a set of UW’s engineered heart tissues (inside the green-topped case at center) riding aboard the International Space Station as part of a test of micro-gravity on heart health. Image courtesy of NASA
There's also a lot to be learned about the how the heart normally functions that can help areas like sports medicine and space travel, says Sniadecki.
Perhaps unsurprisingly, years of training has a significant effect on the size and structure of an athlete’s heart. Heart problems are also the leading cause of death for young athletes, often because of heart conditions they aren’t yet aware of. Understanding more about the strain that athletes put on their hearts might allow them to train more safely and effectively.
Related story
Hearts in space
And what about the effects of micro-gravity? Spaceflight is known to have harmful impacts on the hearts of astronauts, so last year the Cell Biomechanics Lab, in partnership with colleagues at Johns Hopkins University and the Tissue Chips in Space program, had a chance to observe their tissues in just those conditions, sending them aboard the International Space Station. Their goal was to try to learn more about what was happens to astronauts’ hearts at a cellular level. Ty Higashi, another of Sniadecki’s graduate students, helped lead the effort.
“The idea of a ‘gentle heart’ has new meaning to me,” says Higashi. “The tissues are incredibly fragile and getting them safely from our lab all the way up to space was definitely a challenge, but I was really happy we pulled it off.”
The little heart cells hung on, surviving the journey to space and, with care from the astronauts aboard, provided heartbeat data for over a month. The team observed a drop in heartbeat force over that time and is analyzing the tissues to look for differences compared to a normal set on Earth.
All these areas represent just a few of the ways the team are hoping their miniature engineered hearts could supply useful new insight.
“The very first stem cell treatment was developed here at UW, so this research really builds on that legacy,” says Sniadecki. “Each time I see these beating tissues, I’m still inspired by the awesomeness of our biology. But I also see a world of possibility there for impacting people’s lives, and that’s the most romantic part of all.”
Learn more
View a lecture by Nate Sniadecki and Ty Higashi about their work modeling cardiac dysfunction in microgravity using engineered heart tissues.
Originally published February 8, 2021